Soap Notes Medical Records
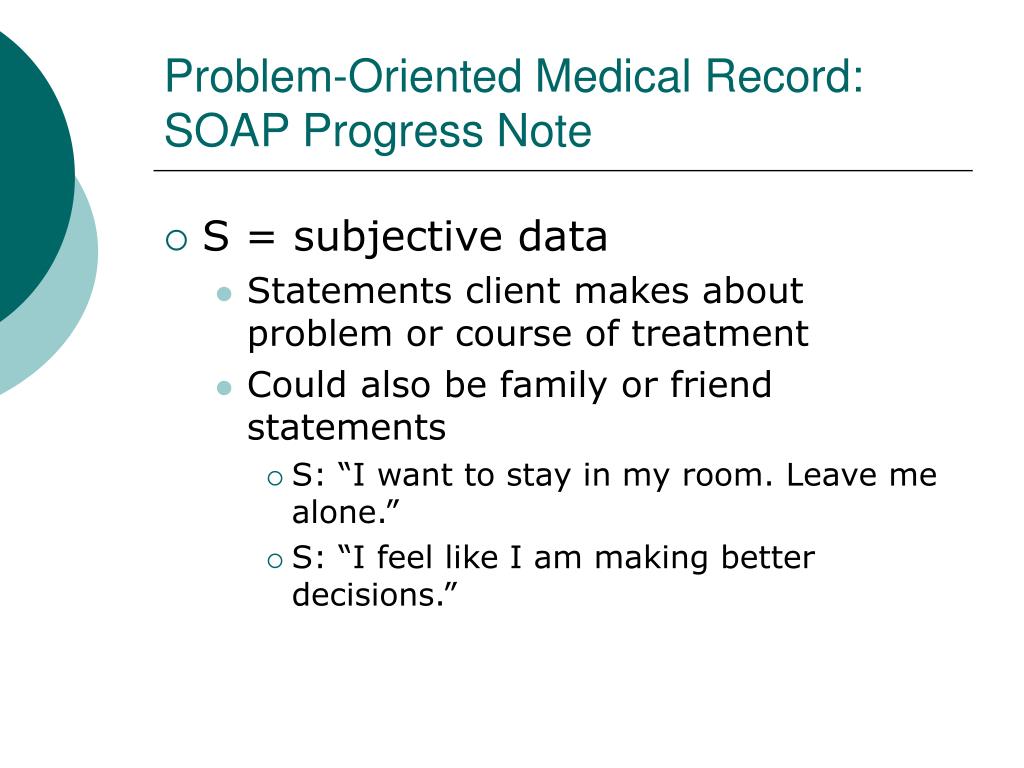
Soap notes is a robust patient manager app that is specifically designed to allow for quick, accurate soap notes for each patient's visit. soap notes is ideal for any person who must manage detailed notes for each patient visit and needs an app that will enter soap notes medical records the notes quickly, and accurately. The soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare providers to write out notes in a patient's chart, along with other common formats, such as the admission note. documenting patient encounters in the medical record is an integral part of practice workflow starting with appointment scheduling, patient check-in and exam. The soap note was first introduced into the medical field by dr. lawrence weed in the early 1970s and was referred to as the problem-oriented medical record (pomr). at the time, there was no standardized process for medical documentation.
Soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health professional[1]. they are entered in the patients medical record by healthcare professionals to communicate information to other providers of care, to provide evidence of patient contact and to inform the clinical reasoning. The soap notes template is an easy and an effective method for quick and proper treatment for a patient. a soap note is usually made up of four divisions, the subjective part that has the details of the patient, the objective part that has the details of the patient that are recorded while he is at the hospital, the assessment part which is. Complying with medical record documentation requirements mln fact sheet page 5 of 6 icn mln909160 january 2021. physical therapy (pt) services documentation did not support certification of the plan of care for physical therapy services. Soap notes are commonly found in electronic medical records (emr) and are used by providers of various backgrounds. generally, soap notes are used as a template to guide the information that physicians add to a patient's emr.
Soapnote How To Write Spotless Healthcare Notes Free
A soap (subjective, objective, assessment, plan) note is a method of documentation used specifically by healthcare providers. soap notes are used so staff can write down critical information concerning a patient in a clear, organized, and quick way. soap notes, once written, are most commonly found in a patient’s chart or electronic medical records. The advent of electronic medical records has not only changed the format of medical records but has increased accessibility of files. the use of an individual dossier style medical record, where records are kept on each patient soap notes medical records by name and illness type originated at the mayo clinic out of a desire to simplify patient tracking and to allow for. Soapnotes an acronym for subjective, objective, assessment and plan is the most common method of documentation used by providers to input notes into patients’ medical records. they allow providers to record and share information in a universal, systematic and easy to read format.
A basic, quality electronic health record system should be able to record soap notes, transfer prescriptions to pharmacists using computerized physician order entry, allow providers to chart without significant impediment, help physicians check treatment recommendations against problem and medication lists, and offer some type of information. Soap notes create a treatment record so you can track the client’s progress towards their therapy goals. this applies if you are a solo massage therapist, or if you are working for a supervising clinician like a physical therapist, chiropractor or medical doctor. some tonic water, bitter lemon, more very light medical notes such as aspirin, then putty, marjoram and hawthorn as well… finish: long, on lemon peel, gentle medical notes, embrocations, smoked olive oil (provided such thing exists, comes handy doesn’t it… yeah, right, no soap whatsoever i think i’ll write a few lines about sample bottles after these notes… anyway, this is tense, on all things apples

2021s Best Medical Software Technologyadvice

How To Write A Soap Note With Soap Note Examples
Best practices: problem-oriented medical record and soap.
Some medical practices may want the fully-written soap note to be reviewed and/or approved by a higher-up, while some practices will want the soap note writer to upload the completed document to a database of medical records. or, the best plan of action may be to carry out the action tasks in the plan as soon as possible. Soap finds its usage in recording patient progress. soap or soap notes as they are widely called also find extensive usage in veterinary practices. it is a way for clinics to record, document, and store patient’s medical information in a systematic way. Documenting a patient assessment in the notes is something all medical students need to practice. this guide discusses the soap framework (subjective, objective, assessment, plan), which should help you structure your documentation in a clear and consistent manner.
Soap Note How To Write Spotless Healthcare Notes Free
• daily notes • date and pt signature • medical information that is readily available in the record • justification for billing services. discharge. follow-up appointments with a: • surgeon • durable medical equipment (dme) medical professional soap notes medical records • mental health practitioner. centers for medicare & medicaid services 37. Shown above is an example of a medical soap note that discusses the present state of a patient who came to the clinic to seek answers for a few complaints. practitioners tend to go into detail with their analysis to gather a sufficient amount of information for their records. 6. nutrition medical soap note.
What is a soap note? examples.

Medical Record Wikipedia
The assessment portion of the note highlights the diagnosis that is specific to this particular visit. often a patient will have several diagnoses; however, in a soap note format, brevity rules, which means often doctors will only dictate soap notes medical records their assessment of the patient's reason for visit on that particular day. Patient records come complete with customisable notes and charting options, patient information history, vital readings and tabulations and diagnostic results all stored intuitively any way you want.
With vetblue, every record contains a history of procedures performed on the animal, as well as drugs or vaccines administered. in addition, users can enter medical and/or instructional notes associated with each patient’s medical record, and these notes can be included on the client’s invoice if desired. Before proceeding, let’s have a brief look at the history of the soap notes. the practice of preparing soap notes began in the 1960s. this was developed by dr. lawrence weed a member of the university of vermont. the purpose of the soap notes was to help in the problem-oriented medical record. now you are asking yourself, why we need soap notes. Progress (soap) notes. progress notes are legal documents. these notes are records of your client’s status and progress. unlike psychotherapy notes, progress notes are read by other staff members to help provide patient care. progress notes should be brief, clear, accurate and hipaa-compliant. maintenance of records and scheduling of appointments, and soap notes all the medical records electronically and above all the billing procedures we
Best practices: problem-oriented medical record and soap notes. september 3, 2015. 0. 0. evidence in integrative healthcare. in 1968, lawrence weed, md, developed the problem-oriented medical record (pomr) “… to develop a more organized approach to the medical record…” (weed l. medical records that guide and teach. nejm vol. 278, no. 11. A soap note template comes in a very structured format though it is only one of the numerous formats health or medical professionals can use. a soap note template by a nurse practitioner or any other person who works with the patient enters it into the patient’s medical records in order to update them.
The soap note stands for subjective, objective, assessment, and plan. this note is widely used in medical industry. doctors and nurses use soap note to document and record the patient’s condition and status. the soap note is considered as the most effective and standard documentation used in the medical industry along with the progress note. Medications and medical allergies. immunization records. such as vaccinations, blood and drug test. other medical encounters. such as hospital admissions, regular checkups, and consultation. to give you more ideas about the finer details of medical notes, just check out our note examples in pdf here. the importance of a medical note. Offers a computer based medical record including templating, soap notes, and patient demographics. Soapnotes are used for admission notes, medical histories and other documents in a patient’s chart. many hospitals use electronic medical records, which often have templates that plug information into a soap note format. most healthcare clinicians including nurses, physical and occupational therapists and doctors use soap notes.
Post a Comment for "Soap Notes Medical Records"